Gastroenterology Tests and Procedures
Our team of physicians are trained in all aspects of gastrointestinal disorders.
After an initial gastroenterology consultation, our doctors may perform procedures including:

The U.S. Preventive Services Task Force recommends that adults age 50 to 75 be screened for colorectal cancer. The decision to be screened after age 75 should be made on an individual basis. Individuals at an increased risk of getting colorectal cancer should talk to their doctor at DDM about when to begin screening, which test is right for them, and how often to get tested. Several screening tests can be used to find polyps or colorectal cancer. This procedure is performed at Mohawk Valley Endoscopy Center.

A colonoscopy/polypectomy may be recommended as a screening test for colorectal cancer. Colorectal cancer is the third leading cause of cancer deaths in the United States. Annually, approximately 150,000 new cases of colorectal cancer are diagnosed in the United States and 50,000 people die from the disease. It has been estimated that increased awareness and screening would save at least 30,000 lives each year. A colonoscopy lets your doctor examine the lining of your large intestine (colon) for abnormalities by slowly advancing a thin flexible tube into your colon. This instrument, called a colonoscope, enables your doctor to visualize images of your colon on a video monitor to detect abnormalities.
To prepare for a colonoscopy, your doctor will tell you what dietary restrictions to follow and what cleansing routine to use. In general, the preparation consists of limiting your diet to clear liquids the day before and consuming either a large volume of a special cleansing solution or special oral laxatives. The colon must be completely clean for the procedure to be accurate and comprehensive, so be sure to follow your doctor’s instructions carefully. A colonoscopy is well-tolerated and rarely causes much pain. You might feel pressure, bloating or cramping during the procedure. Typically, your doctor will give you a sedative or painkiller to help you relax and better tolerate any discomfort. You will lie on your side or back while your doctor slowly advances a colonoscope along your large intestine to examine the lining. Your doctor will examine the lining again as he or she slowly withdraws the colonoscope. The procedure itself usually takes less than 45 minutes, although you should plan on two to three hours for waiting, preparation and recovery. In some cases, the doctor cannot pass the colonoscope through the entire colon to where it meets the small intestine. Your doctor will advise you whether any additional testing is necessary. This procedure is performed at Mohawk Valley Endoscopy Center.

An upper endoscopy helps your doctor evaluate symptoms of upper abdominal pain, nausea, vomiting or difficulty swallowing by allowing your doctor to examine the lining of the upper part of your gastrointestinal tract, which includes the esophagus, stomach and duodenum (the first portion of the small intestine). Your doctor will use a thin, flexible tube called an endoscope, which has its own lens and light source, and will view the images on a video monitor. To prepare for an upper endoscopy, an empty stomach allows for the best and safest examination, so you should have nothing to eat or drink, including water, for approximately six hours before the examination. Your doctor will tell you when you should start fasting as the timing can vary.
At the start of the upper endoscopy, the doctor might start by spraying your throat with a local anesthetic or by giving you a sedative to help you relax. You’ll then lie on your side, and your doctor will pass the endoscope through your mouth and into the esophagus, stomach and duodenum. The endoscope doesn’t interfere with your breathing. Most patients consider the test only slightly uncomfortable, and many patients fall asleep during the procedure. An upper endoscopy is also referred to as a EGD or Gastrocopy. This procedure is performed at Mohawk Valley Endoscopy Center.


In people who have cirrhosis, high pressure in the veins that carry blood from the intestines to the liver (portal hypertension) causes many problems. Variceal bleeding—bleeding from enlarged veins (varices) in the digestive tract—is an extremely serious complication of portal hypertension. For people who have advanced cirrhosis and varices, especially in the esophagus, the risk of variceal bleeding is high. After varices have bled the first time, there is a high risk of bleeding again. The chance of bleeding again is highest right after the first bleed stops. Then the chance of bleeding again gradually goes down over the next several weeks. If varices are not treated, bleeding can lead to death.
During variceal banding, a doctor uses an endoscope to place an elastic ring that looks like a rubber band around an enlarged vein. Banding the vein in this manner will cut off blood flow through the vein. It may be difficult to use this procedure while someone is actively bleeding, because the device used to place the bands obscures the doctor’s vision.
Variceal banding has been shown to be as effective as sclerotherapy in treating episodes of bleeding, and it has fewer complications. Variceal banding is often done several times to control the varices and prevent bleeding. For example, banding might be repeated every 2 to 4 weeks for 3 to 4 sessions. Your doctor will monitor (check) the varices every 3 to 12 months after that for the rest of your life.

FibroScan ® is a non-invasive test that helps assess the health of your liver. Specifically, it uses ultrasound technology to determine the degree of fibrosis or scarring that may be present in your liver from various liver diseases or conditions. It measures fibrosis (scarring) and steatosis (fatty change) in your liver. Fatty change is when fat builds up in your liver cells.

Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (esophagus). This backwash (acid reflux) can irritate the lining of your esophagus.
The most common symptom of GERD is heartburn, a condition that 20 percent of American adults experience at least twice a week. Although these individuals are at increased risk of developing esophageal cancer, the vast majority of them will never develop it. But in a few patients with GERD (estimated at 10-15%), a change in the esophageal lining develops, a condition called Barrett’s esophagus.
Doctors believe most cases of adenocarcinoma of the esophagus begin in Barrett’s tissue.
Barrett’s esophagus is a condition in which the esophageal lining changes, becoming similar to the tissue that lines the intestine. A complication of GERD, Barrett’s it is more likely to occur in patients who either experienced GERD first at a young age or have had a longer duration of symptoms. The frequency and or severity of GERD does not affect the likelihood that Barrett’s may have formed. Dysplasia, a precancerous change in the tissue, can develop in any Barrett’s tissue. Barrett’s tissue is visible during endoscopy, although a diagnosis by endoscopic appearance alone is not sufficient. The definitive diagnosis of Barrett’s esophagus requires biopsy confirmation.
Your doctor will first perform an upper endoscopy to diagnose Barrett’s esophagus. Barrett’s tissue has a different appearance than the normal lining of the esophagus and is visible during endoscopy. Although this examination is very accurate, your doctor will take biopsies from the esophagus to confirm the diagnosis as well as look for the precancerous change of dysplasia that cannot be seen with the endoscopic appearance alone. Taking biopsies from the esophagus through an endoscope only slightly lengthens the procedure time, causes no discomfort and rarely causes complications. Your doctor can usually tell you the results of your endoscopy after the procedure, but you will have to wait a few days for the biopsy results.
Barrett’s esophagus is twice as common in men as women. Even in patients with heartburn, Barrett’s esophagus is uncommon and esophageal cancer is very rare. One recommendation is to screen patients older than 50 who have had significant heartburn or required regular use of medications to control heartburn for several years.

Hemorrhoidal banding is a non-surgical method for treating and removing hemorrhoids. Hemorrhoids are swollen vessels in the lower rectum and anus caused by increased pressure or straining. While not life threatening, hemorrhoids can cause bleeding, burning or discomfort.
For decades, chronic hemorrhoid sufferers resorted to surgery for relief. Today, a procedure called the CRH-O’Regan Disposable Hemorrhoid Banding System has all but eliminated the need for surgery and allows patients to be treated quickly and resume normal activity with very little discomfort.
Most patients with office jobs find they can return to work the same day. The O’Regan method uses a small rubber band to strangle the base of the swollen vein, which cuts off the blood supply to the hemorrhoid. This causes the banded tissue to shrink and fall off along with the rubber band. Typically, this happens within a few days after your appointment during a routine trip to the toilet, and you may not even notice when this happens. The treatment itself takes less than five minutes and can be performed in one of our offices or endoscopy centers.
Our physicians trained in this procedure tend to avoid doing more than one treatment per visit. Subsequently, some patients who have multiple hemorrhoids may require two or three treatments which are scheduled a few weeks apart.
The band placement is relatively painless due to this refined technique and it does not require anesthesia or other numbing agents. You may experience a dull ache or sense of fullness in the rectum within the first 24 hours, but this can generally be relieved by over-the-counter pain medication.

The Digestive Disease Medicine Infusion Center offers comprehensive IBD infusion therapy in a clean comfortable environment. Our state of the art five chair infusion suite is designed for patients that require scheduled infusions. Your doctor may recommend that you try infusions of medications called biologics as a treatment for Crohn’s disease. or Ulcerative colitis. This method usually involves using a needle or catheter. Ideally, these infusions can help keep the condition in remission.
When an infusion is prescribed, a RN Infusion Nurse with IBD experience is present during each infusion.

PEG stands for percutaneous endoscopic gastrostomy, a procedure in which a flexible feeding tube is placed through the abdominal wall and into the stomach. PEG allows nutrition, fluids and/or medications to be put directly into the stomach, bypassing the mouth and esophagus.
Stomach polyps — also called gastric polyps — are masses of cells that form on the lining inside your stomach. These polyps are rare and usually don’t cause any signs or symptoms. Stomach polyps are most often discovered when your doctor is examining you for some other reason.
Most stomach polyps don’t become cancerous. But certain types can increase your risk of stomach cancer in the future. Depending on the type of stomach polyp you have, treatment might involve removing the polyp or monitoring it for changes. This procedure is performed at Mohawk Valley Endoscopy Center.

Capsule Endoscopy lets your doctor examine the lining of the middle part of your gastrointestinal tract, which includes the three portions of the small intestine (duodenum, jejunum, ileum). Your doctor will give you a pill sized video camera for you to swallow. This camera has its own light source and takes pictures of your small intestine as it passes through. These pictures are sent to a small recording device you have to wear on your body.
Your doctor will be able to view these pictures at a later time and might be able to provide you with useful information regarding your small intestine.

An abdominal CAT or CT scan is an imaging method that uses x-rays to create cross-sectional pictures of the belly area.
This noninvasive diagnostic imaging procedure uses a combination of X-rays and computer technology to produce horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, organs, and blood vessels. CT scans are more detailed than standard X-rays.
CT scans may be done with or without “contrast.” Contrast refers to a substance taken by mouth or injected into an intravenous (IV) line that causes the particular organ or tissue under study to be seen more clearly. Contrast examinations may require you to fast for a certain period of time before the procedure. Your doctor will notify you of this prior to the procedure.

Ultrasound imaging of the abdomen uses sound waves to produce pictures of the structures within the upper abdomen. It is used to help diagnose pain or distention (enlargement) and evaluate the kidneys, liver, gallbladder, bile ducts, pancreas, spleen and abdominal aorta.A gastrointestinal ultrasound is a practical and safe diagnostic tool in inflammatory bowel disease that is global prominence amongst clinicians.

Although an endoscopy provides an accurate means by which to identify structural or histologic abnormalities of the gastrointestinal (GI) tract, there remains a need for simple, noninvasive, less expensive tests that can provide similar or supplemental information to endoscopy. Several breath tests have been developed to provide help supplemental information to an endoscopy.
A hydrogen breath test is used to detect lactose intolerance lactose intolerance (inability to digest lactose, the sugar found in milk), as well as fructose or sucrose intolerance. A hydrogen breath test can also detect bacterial overgrowth in the small intestine (a condition in which the normal flora of the intestine is altered; affects absorption of nutrients). Testing is performed at our office.
The urea breath test is a simple breath test that detects the presence of Helicobacter pylori, a bacteria found in the stomach. H. pylori has been found to cause peptic ulcers in some patients, while others show the presence of H. pylori with no symptoms at all.
 The 48-Hour Bravo ™ Esophageal pH Test assess whether acid is coming back into the esophagus from the stomach causing pain, nausea, heartburn, and chest pain. This test involves placing a pH capsule approximately the size of a gelcap to the esophageal wall with the use of an endoscope. The procedure to place the capsule through an upper endoscopy is done under conscious sedation. For the duration of the test, you will keep a diary of any symptoms you experience and record exact times for when you eat and when you are lying down.
The 48-Hour Bravo ™ Esophageal pH Test assess whether acid is coming back into the esophagus from the stomach causing pain, nausea, heartburn, and chest pain. This test involves placing a pH capsule approximately the size of a gelcap to the esophageal wall with the use of an endoscope. The procedure to place the capsule through an upper endoscopy is done under conscious sedation. For the duration of the test, you will keep a diary of any symptoms you experience and record exact times for when you eat and when you are lying down.
The capsule naturally falls off the wall of the esophagus and passes through your digestive tract and eliminated from the body.
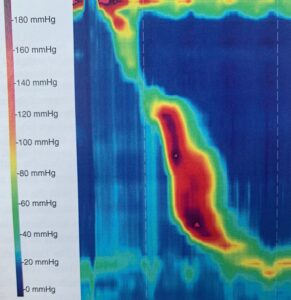
High resolution impedance manometry (HRIM) measures pressures and fluid movement in the esophagus and lower esophageal sphincter. These measurements enable diagnosis of esophageal motility disorders and are crucial to the planning of most esophageal surgery. HRIM procedure is performed in our office where a small flexible catheter (tube) will be placed into your esophagus through your nose (after applying local anesthetic to the nose). You will be asked to swallow small amounts of salt water 10-12 times during the test. The test lasts about 10-15 minutes in most instances.

Radiofrequency ablation (RFA) uses heat to remove precancerous tissue from the esophagus. Barrett’s esophagus patients treated with radiofrequency ablation are less likely to progress to esophageal cancer compared to patients who undergo surveillance. Untreated Barrett’s may lead to esophageal adenocarcinoma, a type of esophageal cancer, so early detection and treatment is critical.

Hepatitis is the inflammation of the liver. It can have many causes,
including viruses, medications and alcohol. Most commonly, however, we
think of the viruses, called A, B and C. Hepatitis A virus causes an acute inflammation of the liver
(hepatitis) that almost always gets better on its own. It can be more
serious if we are older when we have the disease. It is easily spread
from person to person, in food and water, and can infect many people at
once
Hepatitis B virus (HBV) can be both acute (short-term illness) and
chronic (ongoing illness), and is spread through blood or other body
fluids in various ways.
Hepatitis C (HCV) is almost always chronic and is spread both sexually and with blood.
Hepatitis A and B can be prevented by vaccination, but not
hepatitis C. Hepatitis C can now be easily treated with medication such as a pill that can be taken over a few months with virtually no side effects .
Contact your doctor for a referral to DDM.

The clinical research unit provides patients with the most advanced level of medical and surgical care, primarily focused on the safe and proven treatment of disorders related to the gastrointestinal tract. DDM is the first gastroenterology practice in Mohawk Valley to integrate research and practice to ensure that our patients are receiving state-of-the art medical care.
Participation in these studies not only provides additional information on how to treat our patients better, it also acts as a guide on what are the best treatments for our community members.
Please feel free to ask your doctor if you would be a good match for our research. There are clear criteria that must be met for participation and we want to make sure you are well informed about any side effects and risks of participating just like any other new medication and procedure you are starting.
If you have questions please contact mjaramillo@ddmcny.com